TB and Parkinson's
Link between tuberculosis and Parkinson’s disease discovered
Published on: 22 May 2018
The mechanism our immune cells use to clear bacterial infections like tuberculosis might also be implicated in Parkinson’s disease, according to a new study.
The findings of the collaborative study led by Newcastle University, the Francis Crick Institute and GSK - published in The EMBO Journal - provide a possible explanation of the cause of Parkinson’s disease and suggest that drugs designed to treat Parkinson’s might work for TB too.
Parkinson’s protein
The most common genetic mutation in Parkinson’s disease patients is in a gene called LRRK2, which makes the LRRK2 protein overactive.
Drugs that block LRRK2 are a promising new treatment for Parkinson’s, with many pharmaceutical companies developing drugs to target LRRK2 and clinical trials underway. But how overactive LRRK2 causes Parkinson’s and why LRRK2 blockers work was a mystery.
The biological causes of Parkinson’s remain largely unknown, making it more difficult to develop and improve treatments. Discovering a mechanism that causes Parkinson’s and how drugs affect it could significantly advance efforts to improve treatments.
Insights from TB
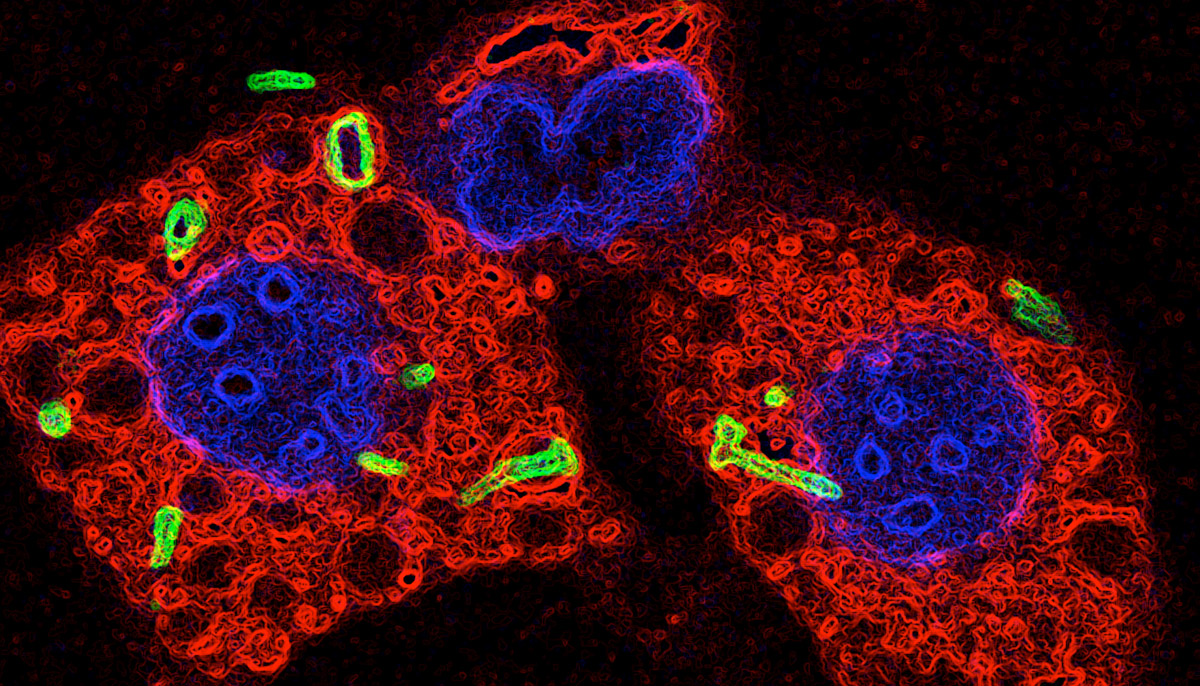
By studying what LRRK2 does in immune cells called macrophages that are infected with Mycobacterium tuberculosis (Mtb) – the bacterium that causes TB – researchers believe they have uncovered a potential cause of Parkinson’s.
Macrophages recognise and engulf Mtb securing it within tight-fitting internal compartments called phagosomes. Another part of the cell called the lysosome then fuses with the phagosome to destroy the bacterium inside.
Using a combination of different experimental approaches, Crick and GSK researchers, in collaboration with Dr Anetta Härtlova and Professor Matthias Trost, from Newcastle University, found that LRRK2 prevents phagosomes from fusing with lysosomes in both human and mouse macrophages, making them less efficient at clearing bacteria. Deleting the LRRK2 gene or treating the cells with an LRRK2 blocker significantly reduced levels of Mtb.
These findings in cells were supported by experiments in mice. When the researchers deleted the gene for LRRK2 in mice, they found that they exhibited an enhanced early immune response to TB infection, and had significantly lower levels of Mtb in their lungs than control mice up to two weeks after infection.
Co-senior author Professor Trost, from Newcastle University’s Institute for Cell and Molecular Biosciences, said: “Both our labs independently identified the main findings and this paper is a great example where sharing data and combining different technologies made the difference.
“Our data implies that the conserved machinery that cells use to destroy and degrade external particles such as bacteria and damaged neurons is an important target for drug discovery.”
Build-up of protein
The team suspect that LRRK2 might be preventing immune cells in the brain from degrading cell debris properly, leading to a build-up of protein in neurons that disrupts their function.
Susanne Herbst, joint first author of the paper and post-doctoral fellow at the Francis Crick Institute, said: “We think that this mechanism might also be at play in Parkinson’s disease, where abnormal masses of protein called ‘Lewy bodies’ build up in neurons in the brain and cause damage.
“By studying TB, we have found a possible explanation for why LRRK2 mutations are a genetic risk factor for Parkinson’s disease. It’s exciting when different fields of research connect up in unexpected ways like this!”
First author, Dr Härtlova, added: "Our work neatly agrees with recent findings that the immune system plays a key role in Parkinson’s disease and other neurodegenerative diseases. Thus, targeting inflammatory responses will be a key goal of Parkinson's disease therapy."
New TB treatments
The findings also suggest that LRRK2 inhibitors could be a powerful new way of combating TB, which kills 1.67 million people every year.
Max Gutierrez, Group Leader at the Crick and senior author of the paper, said: "Drug-resistant TB is a serious emerging problem, and boosting the body’s own immune defence against TB is an important step in the battle against antibiotic resistant strains.
"LRRK2 inhibiting drugs are already being developed to treat Parkinson’s disease and we’re trying to see if we can repurpose them as a potential new TB therapy. This should be relatively straightforward because TB infects the lungs, so the LRRK2 inhibitors wouldn’t need to cross the blood-brain barrier like they do in Parkinson’s disease.”
Reference
LRRK2 is a negative regulator of Mycobacterium tuberculosis phagosome maturation in macrophages
Anetta Härtlova, Susanne Herbst, Julien Peltier, Angela Rodgers, Orsolya Bilkei-Gorzo, Antony Fearns, Brian D. Dill, Heyne Lee, Rowan Flynn, Sally A. Cowley, Paul Davies, Patrick A. Lewis, Ian G. Ganley, Jennifer Martinez, Dario R. Alessi, Alastair D. Reith, Matthias Trost, and Maximiliano G. Gutierrez
The EMBO Journal: 10.15252/embj.201798694
Press release adapted with thanks to The Francis Crick Institute



