Microbes in Health and Disease
Investigating microbial interactions in human hosts.
Microbes are the most abundant and diverse organisms on earth. They are capable of occupying a plethora of ecological niches. The human body is a collection of distinct environments, where commensal and pathogenic organisms interact in unique ways to benefit health or cause disease.
We aim to understand the molecular basis of these interactions, with particular focus on:
- how gut bacteria breakdown dietary fibre
- structure, function and regulation of diverse protein secretion systems
- competition between commensals and pathogens for host colonisation
- microbe-host interaction
- virulence determinants in prokaryotic and eukaryotic pathogenic microbes
- how pathogens regulate gene expression
- how bacteria develop antimicrobial resistance
- nutrient transporters and symbiosis
Research Impact
Our work directly relates to real-world problems in infectious diseases, gut health and antimicrobial resistance by investigating the fundamental basis of diverse host-microbe interactions.
Our research builds on the strong reputation of basic microbiological research at Newcastle. Members of our theme have secured funding and PhD studentships from major sources including:
- Wellcome Trust
- MRC
- BBSRC
- UKRI
- Royal Society
- Academy of Medical Sciences
- The Lister Institute
- The EU and ERC
- The UK Government (DEFRA)
Research Areas
Our research is focused on studying the basis of host-microbe interactions. We study the mechanisms that pathogenic and commensal microbes use to occupy diverse host niches. We aim to exploit our discoveries for the development of novel anti-infectives, and we also study how microbes develop resistance to existing antibiotics. Through these approaches we are tackling the global problem of antimicrobial resistance.
Gut pathogens and the microbiota
Interactions between microbes and the gut impact on several aspects of human health. We study the molecular physiology of anaerobic bacteria, such as how commensal species such as Bacteroides breakdown carbohydrates consumed in our diet to maintain gut homeostasis. We also study the energetics of anaerobic respiration and fermentation in commensal species such as Escherichia coli. In addition, we investigate the potential of probiotic bacteria in gut health.
We investigate how pathogens overcome host defences and colonise the gut. We study how bacteria, such as Escherichia coli, Salmonella enterica and Clostridioides difficile regulate virulence gene expression and interact with host cells at the molecular level and make dormant cells to cause infections. We study how commensal fungi, such as Candida albicans, responds to environmental cues and host immune defences found in the gastrointestinal tract. We also study the impact of polymicrobial infections on the microbiome.
Contacts
Skin and oral host-microbe interactions
Host–microbe interactions play a critical role in maintaining health and driving disease in both the skin and oral cavity. Numerous inflammatory disorders are now linked to microbiome dysbiosis or infection at these tissue sites.
In the oral cavity, bacteria and fungi have a major impact on health, with dental plaque formation leading to gum disease. We study how organisms such as Streptococci form biofilms and communicate within this niche, and we investigate the host inflammatory response to mucosal colonisation by microbes such as Candida albicans. This fundamental knowledge is also being translated into strategies to control biofilms and prevent oral disease.
The skin is another dynamic microbial habitat where bacteria, fungi, and viruses coexist with the host barrier and immune system. Disruptions in these communities contribute to inflammatory diseases such as atopic dermatitis, acne, ichthyosis, dandruff, and dry skin. Many interactions are highly site-specific—for example, scalp disorders often involve hair follicle microbes, while underarm and toe-web niches are associated with body odour and localised infections. Our research focuses on how organisms such as Staphylococcus, Cutibacterium, and Malassezia interact with the epidermis to drive inflammation and barrier dysfunction. We employ sequencing, strain-level analysis, and advanced skin models to identify microbial mechanisms and uncover new therapeutic opportunities.
Together, our work on skin and oral health provides complementary insights into host–microbe interactions and links directly to the NIHR Newcastle Biomedical Research Centre’s Skin Disease and Oral Disease programme.
Contacts
Nasal and respiratory pathogens
The skin is normally colonised by unique members of the microbiota. We study how the opportunistic pathogen Staphylococcus aureus outcompetes these microbes to colonise the nasal cavity.
Pseudomonas aeruginosa is a multidrug resistant pathogen associated with respiratory infection. We study how it scavenges iron to support this process
Mycobacterium tuberculosis is one of the top 10 causes of death. We are particularly interested in antimicrobial resistance, transport processes and modes of action of anti-tubercular agents. Additionally, we investigate how S. aureus, Pseudomonas aeruginosa and Mycobacterium abscessus cause potentially life-threatening infection of the cystic fibrosis lung.
Contacts
Infection of the urinary tract and bloodstream
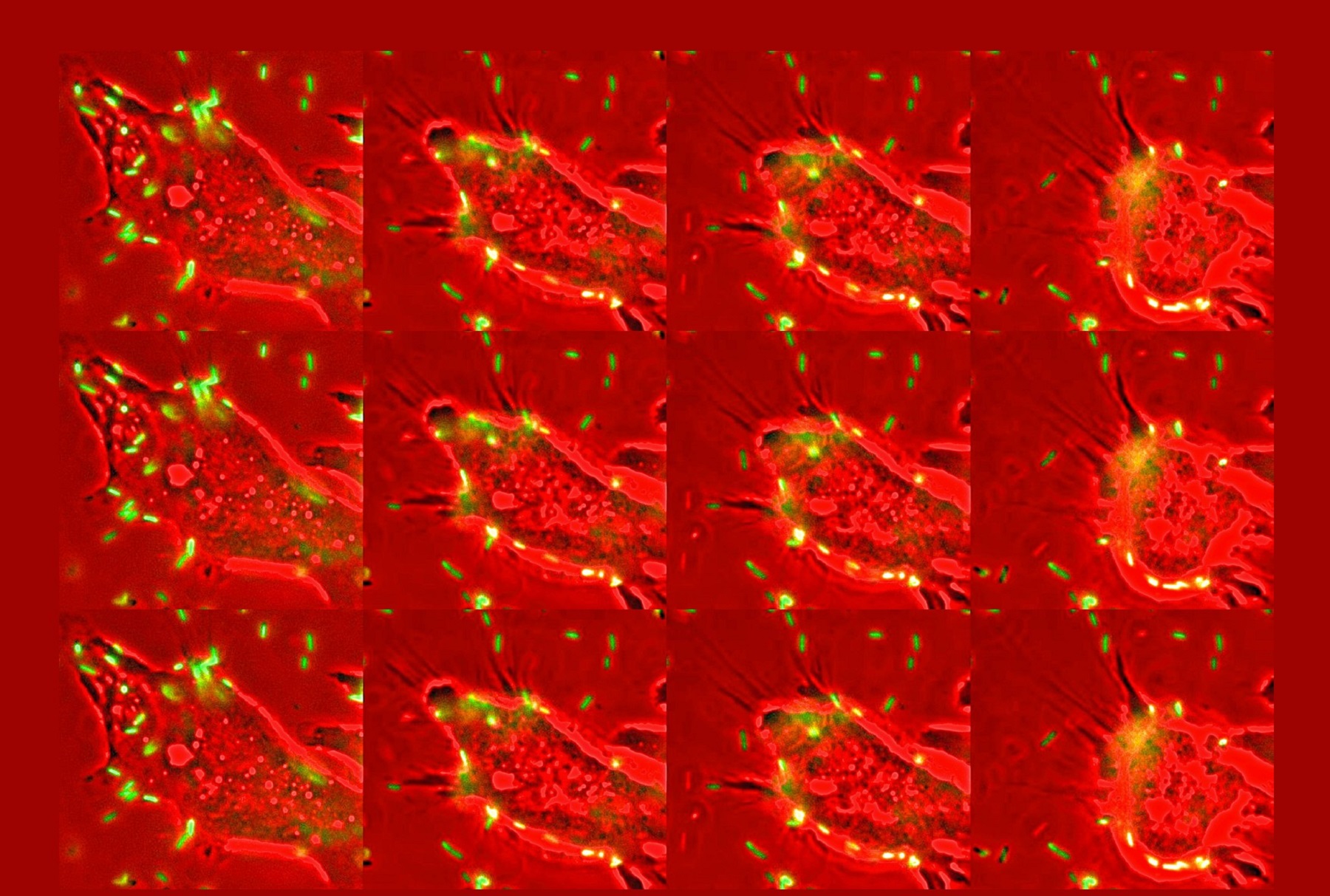
Infection of the Urinary Tract is a major clinical problem worldwide and often associated with antimicrobial resistance. We investigate molecular interactions between uropathogens, such as E. coli, and the vaginal or bladder epithelia. We have particular expertise in L-form bacteria, and study how they evade antibiotic killing and form in vivo. Additionally, we research how the fungal pathogen C. albicans adapts to host-imposed stress.
Extraintestinal pathogens can often invade the bloodstream and disseminate systemically, potentially causing lethal sepsis. We study how E. coli and C. albicans adapts to and survives in the systemic environment during episodes of bacteraemia or candidemia.
Contacts
Microbial-host symbiosis
- glycan foraging by Bacteroides
- chitin metabolism by Serratia marcescens
- the role of bacterial sphingolipids in host colonisation and signalling by Bacteroides and other gut microbes
Contacts
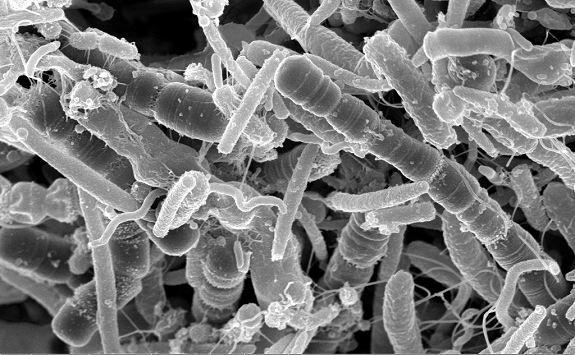
Molecular mechanisms of antimicrobial resistance
Antimicrobial-resistant infections are a rapidly growing cause of morbidity and mortality. Predictions indicate that within a few decades, mortality arising from infection by drug-resistant pathogens may surpass those from cancer and diabetes combined. We study how microbes acquire and maintain resistance, both in the laboratory setting and during infection. We use approaches including biochemistry, genetics, microfluidics, microscopy, cellular and structural biology to decipher mechanisms by which bacteria and fungi evolve resistance and evade drug toxicity. The knowledge we generate establishes the foundation for preventing the development of resistance and for effectively targeting antimicrobial-resistant pathogens.
Contacts
Natural Product Drug Discovery & Screening
Bacterial natural products (specialised metabolites) comprise more than half of all clinically used antibiotics, most of which were discovered in the pre-genomics age. In fact, genome sequencing has since revealed that only 3% of the pathways encoded in their genomes (biosynthetic gene clusters, BGCs) have been matched to molecules. Since the majority of bacterial BGCs have no known product, and most molecules have no linked BGC, genome mining must be combined with unbiased metabolomics data to enable these links to be made. We study bacteria using a combined ‘omics strategy (genomics, transcriptomics, metabolomics) with computational and laboratory screening approaches to understand what influences bacterial chemistry with the focus on drug discovery, in particular antibiotics.
Contacts
Research Culture
We provide a dynamic and supportive environment for all our members across all career stages. We provide mentorship and help with grant applications and paper submissions. We are active participants in the Biosciences Institute early career mentoring programme led by theme member Jan Quinn. We assist our ECRs with fellowship choices, applications, and interview preparation. We have PGR and post-doc leads to ensure that our ECR views are well represented.
ECR Lead: Henrik Strahl
PGR Lead: Natalia Los and Chloe Ellison
Post-doc Lead: Rachel Darnell and Jean-Lou Reyre
We are committed to Equality Diversity and Inclusion and promote EDI practices in all that we do. This includes family-friendly flexible working arrangements and family-friendly meeting times.
EDI Leads: Katharina Trunk and Javier Abellon-Ruiz
We host a weekly seminar series to allow members to share their research progress in an informal and supportive setting. Postgraduate students, researchers and technicians are all encouraged to take part.
We are committed to engaging with the next generation of microbiologists and work alongside the School of Biomedical, Nutritional and Sport Sciences and the FMS Graduate School to provide research-led teaching in microbiology and host-pathogen interactions.