Precision Medicine, Genomics and Informatics
We aim to improve treatments to benefit patients and enhance health and wellbeing. We achieve this by exploiting multidimensional clinical, genetic, pathological and molecular data.
Precision medicine is the optimal delivery of health care to individuals and populations. It embraces stratified, structured and relevant approaches to health and wellbeing. These must be predictive, preventative, personalised and participatory. We use our collective expertise to improve patient and population health. We deliver precision medicine using:
- high dimensional datasets
- innovative methods including wearable technologies and mobile applications
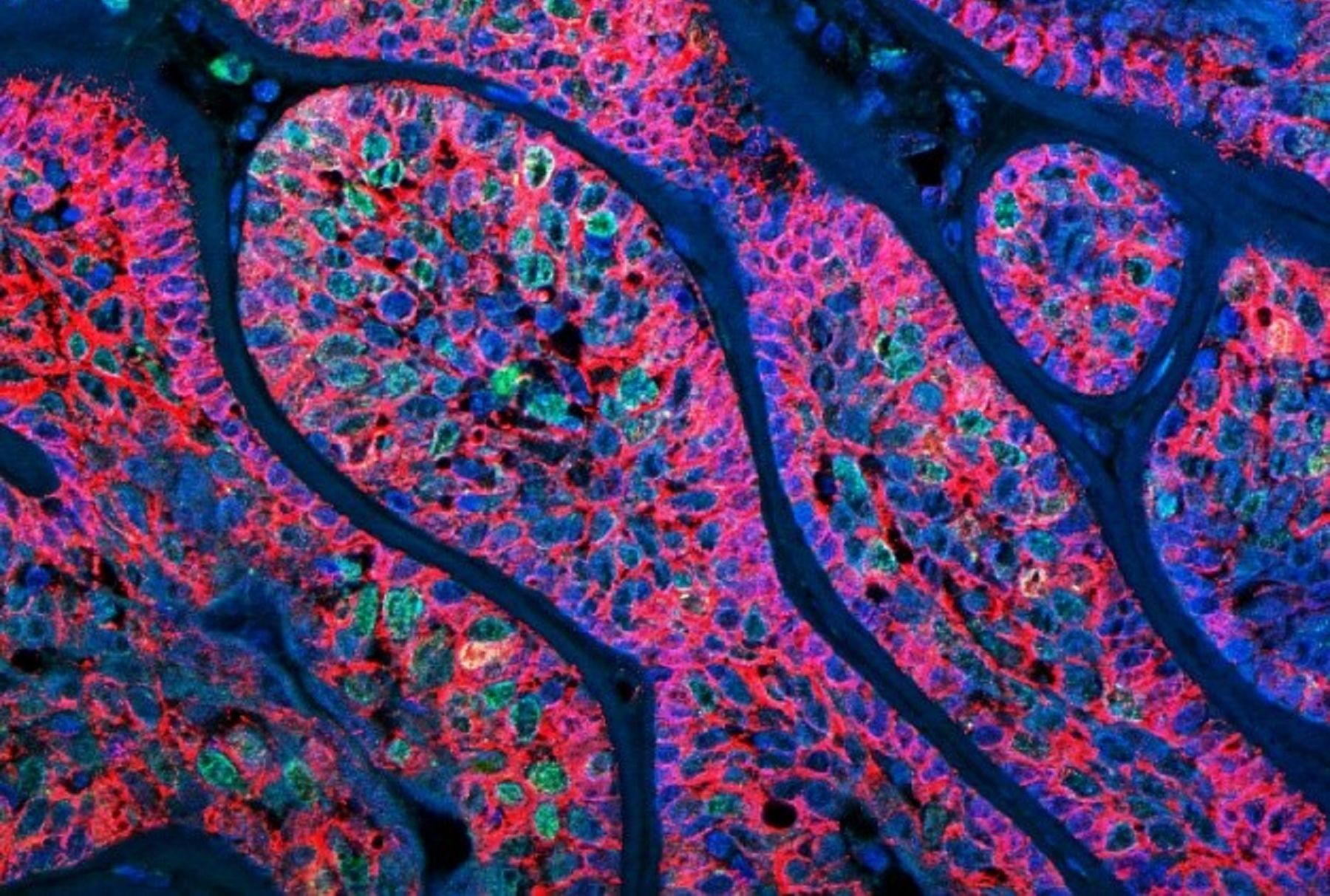
- bespoke laboratory technologies such as next generation sequencing, patient-derived organoids and gene editing.
Precision medicine is at the core of high quality service provision by NHS partners, particularly in Newcastle Health Research Partnership (NHRP) and Diagnostics North East. Close links with clinical teams allow translation into patient benefit quickly and efficiently. This includes biomarkers for tailored treatment and pharmacogenomic stratification to optimise drug efficacy and safety. Encouraging engagement with the public and our students is essential for this translation.
Linking with other university groups enriches our ability to analyse complex data. Enabling the development of innovative methods such as artificial intelligence and deep learning. These groups include:
- Innovation Methodology and Application research theme
- Discovery of Medicines research theme
- School of Computing
Our core members have specific expertise in three main disease clusters:
- chronic non-communicable diseases
- rare diseases
- oncology
Chronic Non-communicable Diseases
Chronic non-communicable diseases have a heavy societal burden worldwide. This encompasses disorders associated with metabolic dysregulation and obesity. Including non-alcoholic fatty liver disease and type 2 diabetes mellitus. A spectrum of immune-driven, inflammatory / degenerative conditions, including chronic skin conditions such as psoriasis. As well as musculoskeletal disorders such as rheumatoid arthritis and osteoarthritis.
Our researchers take a systems biology approach to these clinical challenges. We use a multi-omic strategy. Identifying novel biomarkers and therapeutic targets in inflammatory and fibrotic conditions. Newcastle plays a leading role in many MRC stratified medicine consortia, including:
Contacts
Rare Diseases
Precision medicine is generating a paradigm shift in our thinking about less common, but no less important conditions. One example is the chronic liver disease, primary biliary cholangitis. In this condition there is a need to identify a subset of patients that are rapid progressors. Newcastle University is a world leader in this condition. Our work has identified new treatment pathways that improve patient outcomes.
Other rare diseases covered by our theme include autoimmune hepatitis. In this condition it is essential to identify non-responders to immunosuppressive treatment. We work on the inherited CYLD cutaneous syndrome which leads to multiple adnexal skin lesions (benign and malignant). We also have interests in ciliopathies, inherited syndromes that impact many organs. Most often leading to chronic lung disease and cystic diseases of the kidneys and liver.
Contacts
Oncology
Precision medicine has had a great impact in oncology. Stratified approaches to cancer therapy are now part of routine clinical care across all age groups. We have a particular interest in malignant melanoma and hepatocellular carcinoma. We have developed novel biomarkers to predict subsequent clinical outcome.
We have developed novel screening assays for colorectal cancer. These are used in both prevention and patient management in high risk groups. We have an international reputation in precision oncology of paediatric solid tumours. This includes both medulloblastoma and neuroblastoma. Our work on molecular classification has helped tailor treatment, improve outcomes and reduce late-effects.
Haematological cancers are responsible for considerable morbidity and mortality. We have developed sophisticated classification models using molecular and clinical markers. Our aim is to develop new treatment methods and improve outcomes for patients. Our work in paediatric leukaemia and lymphoma has led to improved methods to identify children at high risk of relapse. This group are now treated more effectively leading to improved survival.
Likewise, our work in adults focuses on understanding how the disease develops at a molecular level. This allows the development of more accurate prognostication models. Leading to more effective treatment strategies with fewer side-effects. These are better tolerated by older patients with co-morbidities.
Our research in precision oncology is part of the Newcastle University Centre for Cancer. It benefits from strong links with industrial partners and other themes in our Faculty. For example, collaboration with Astex Pharmaceuticals and Janssen Pharmaceutica led to the development of Erdafitinib. An oral pan-FGFR inhibitor. It is approved for adult urothelial carcinoma with susceptible FGFR mutations.
Linked research themes include:
Contacts
Methods and Technologies
Success in precision medicine relies on generating data from a range of methodologies and platforms. These include:
- cytogenetics
- genomics, pharmacogenomics and other ‘omics’
- translational therapeutics
- toxicology
- computational pathology
We can then integrate and mine these huge data sets. Utilising our expertise in bioinformatics and our processing capacity in high performance computing. Researchers in our theme continue to develop and enhance such cutting edge technologies in their own right. At the same time providing fundamental support to the disease specific groups in our theme. We are world leaders in the genetics of complex disease, an area inextricably linked to bioinformatics.
The theme contributes to and benefits from links to the Faculty Central Facilities:
- Bioimaging Unit
- Bioinformatics
- Flow Cytometry Unit
- Genomics
- Newcastle Biobank
- MRC Molecular Pathology Node
- NIHR Newcastle In Vitro Diagnostics Co-operative