Immunity and Inflammation
We study immunity and inflammation across the life-course, in health and disease.
We are a diverse group of researchers from both clinical and scientific backgrounds. Our shared vision is to improve human health by delivering the highest quality research, education, and outreach activities.
Our research embraces normal and pathologic development, activity, and homeostasis of the immune system. By studying the mechanisms of protective immunity and immune-mediated inflammatory disease, our work informs diagnosis, stratification, and treatment.
We collaborate widely across the university and beyond, including with industry and the public. We have a high proportion of clinically active academics and work closely with NHS partners on both research and clinical service provision. For example, the National Renal Complement Therapeutics Centre is an umbrella for both clinical care and research into complement disorders.
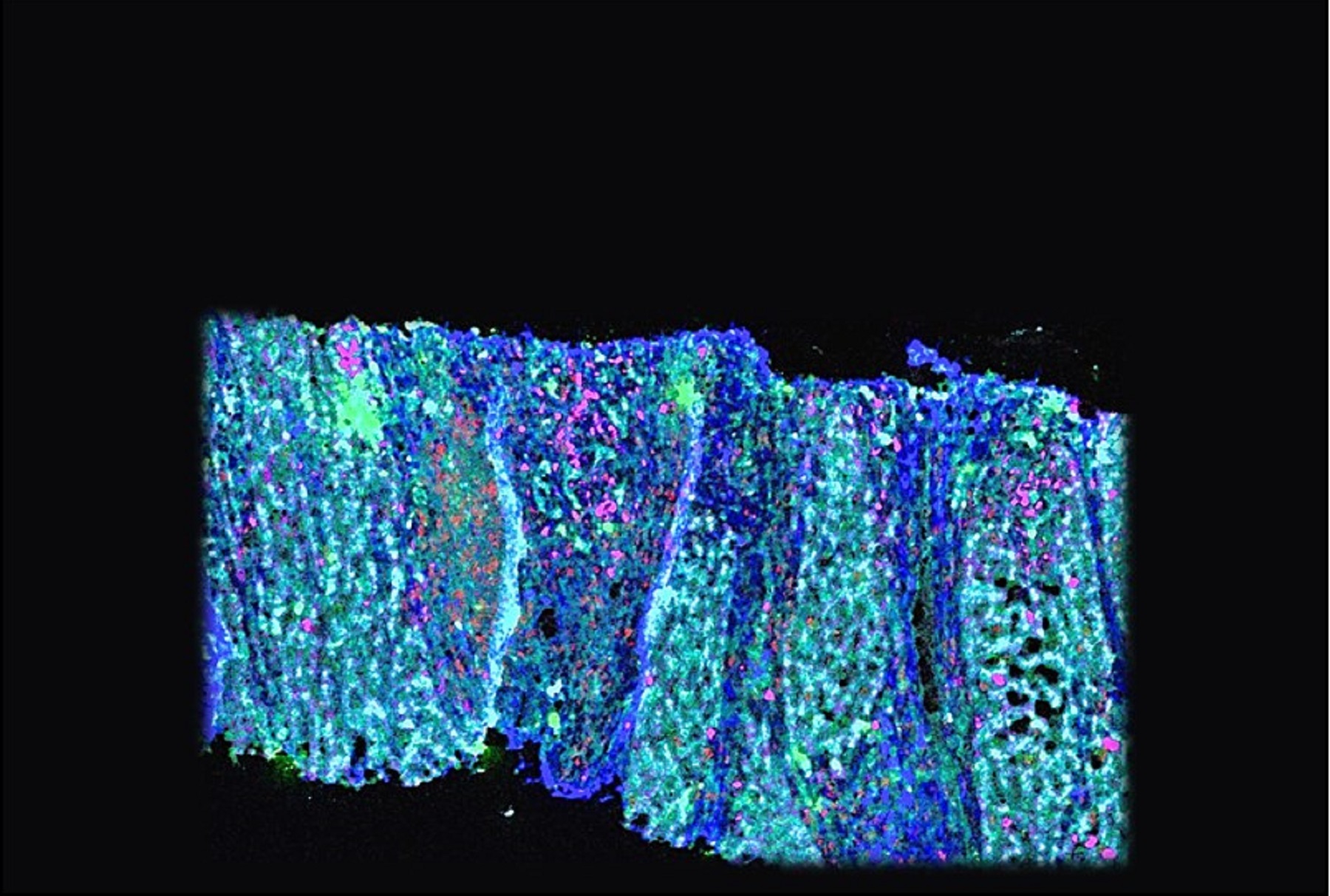
Immunopoiesis and Immunomics
We study the development and diversification of immune cells of different types and function, especially in humans. We use state-of-the-art methods, including single cell ‘omics and in vitro modelling of haematopoiesis.
We work in partnership with excellent Newcastle University facilities, the NHS and collaborative consortia. We tackle a number of research questions, such as:
- how and why does the immune cell content of tissues vary?
- what are the molecular signatures of infection or immune-mediated disease states and which cells confer them?
- what can we learn about the healthy development and function of the immune system from blood cancers and inborn errors of immunity?
Contacts
- Venetia Bigley
- Matthew Collin
- Marieke Emonts-le Clercq
- Andrew Filby
- Andrew Gennery
- Sophie Hambleton
- Muzlifah Haniffa
- Martin Howell
- Laura Jardine
- Rebecca Payne
Tolerance and immune dysregulation
Our research on immune dysregulation covers the full spectrum of scientific investigation. From basic science through observational studies to first-in-man clinical trials. We study auto/alloimmunity including the following:
- rheumatological: rheumatoid arthritis, Sjögren’s syndrome, vasculitis
- endocrine: Graves’, Addison’s disease
- gastrointestinal - inflammatory bowel disease
- inborn errors of immunity presenting as immune dysregulation
- autoimmunity as a complication of cancer immunotherapy
- graft rejection and graft-versus-host disease
Some of the research topics we work on include:
- what are the cellular and molecular mechanisms that maintain tolerance to self-antigens
- can tolerance be induced after autoimmune disease or transplantation and how can we measure this
- can we use this knowledge to restore therapeutic tolerance with precision medicine and so withdraw other forms of immunosuppression
- why do patients with autoimmune disease experience fatigue and can we target this therapeutically
Contacts
- Amy Anderson
- Ken Baker
- Matthew Collin
- Christopher Duncan
- Aisling Flinn
- Andrew Gennery
- Sophie Hambleton
- Catharien Hilkens
- John Isaacs
- Laura Jardine
- Chris Lamb
- Fai Ng
- Simon Pearce
- Christopher Stewart
Tumour Immunology
We are interested in the pathogenic role of chronic inflammation in neoplastic transformation, for example the origins of liver cancer. Our researchers study the role of immune cells in the tumour microenvironment and anti-tumour immunity:
- what controls the balance between immune activation and tolerance towards tumours. How is this impacted by chronic infections and immune stimulants
- in innate cells what mechanisms contribute to or hinder anti-tumour immunity
- to what extent does immune dysregulation after checkpoint inhibitor therapy resemble spontaneous autoimmune disease
- how does the tumour microenvironment support tumour growth e.g. cutaneous T cell lymphoma and liver cancer
Contacts
Inflammation and Infection
Inflammation is a fundamental protective mechanism. It occurs when cells and tissues react to harmful stimuli such as pathogens or tissue damage. Either too much or too little inflammation is associated with disease. Unravelling this complexity will inform the development of novel biomarkers and therapeutics.
II researchers in this field focus on the following research areas:
- how do different cell types contribute to protective and pathological inflammation in tissues? For example, the lung in COVID-19 or cystic fibrosis. The gut in inflammatory bowel disease, inflammatory skin disease, and the transplanted kidney
- the molecular basis of complement dysregulation and how can we restore homeostasis
- how does the microbial flora - microbiome - modulate barrier integrity and immune responses at body surfaces
- the relationship between local and systemic immune activation
- how cells respond to invasion by intracellular pathogens
- what can inborn errors teach us about the pros and cons of inflammation
- do pre-existing chronic conditions and their therapy impact host responses to infection
Contacts
- Simi Ali
- Malcolm Brodlie
- Christopher Duncan
- Andrew Filby
- Andrew Gennery
- Sophie Hambleton
- Muzlifah Haniffa
- Iram Haq
- Christopher Harding
- Claire Harris
- Thomas Hellyer
- David Kavanagh
- John Kirby
- Chris Lamb
- Kate Madden
- Kevin Marchbank
- Kate Musgrave
- Christopher Nile
- Johan Panek
- Rebecca Payne
- Jason Powell
- Anthony Rostron
- Neil Sheerin
- John Simpson
- Christopher Stewart
- Alison Tyson-Capper
- Christopher Ward
- Polina Yarova
Research culture
Members of our theme actively participate in research-led teaching as a core activity. We offer a rich and supportive training environment for students and researchers over the stages of their studies/careers.
Theme members Desa Lilic and Mario Abinun have set up a fund to nurture interactions between Newcastle University and Serbian immunologists and clinical immunologists.
Find out more about the Serbian Clinical Immunology Fund.
Steering Committee
We are a diverse theme with members from different backgrounds and professional specialties. It is important that all our members feel represented and this is reflected in the make-up of our steering committee. Members include:
- Theme Lead: Matthew Collin
- Deputy Theme Leads: Catharien Hilkens
- Teaching Leads: Lei Huang
- Early Career Researcher Leads: Christopher Duncan
- EDI Leads: Rebecca Payne, Simi Ali
- Technician Representative: Sarah Pagan
- Professional Services Representative: